Dermal Fillers: Classification, Risks, and Management of Side Effects & Adverse Effects
Faramarz Rafie M.D. / Vancoderm Academy (VDA) / Vancoderm Clinic (VDCmed.com)
At Vancoderm Academy, we are committed to equipping medical practitioners with the knowledge and skills necessary to deliver safe and effective aesthetic treatments. Dermal filler injections require not only technical precision but also a deep understanding of their potential side effects and complications. In British Columbia, only registered and licensed medical professionals are authorized to perform these procedures, reflecting the importance of professional expertise. This training-focused blog post will review the possible adverse effects of dermal fillers, highlight key safety considerations, and emphasize best practices to help practitioners minimize risks and optimize patient outcomes.
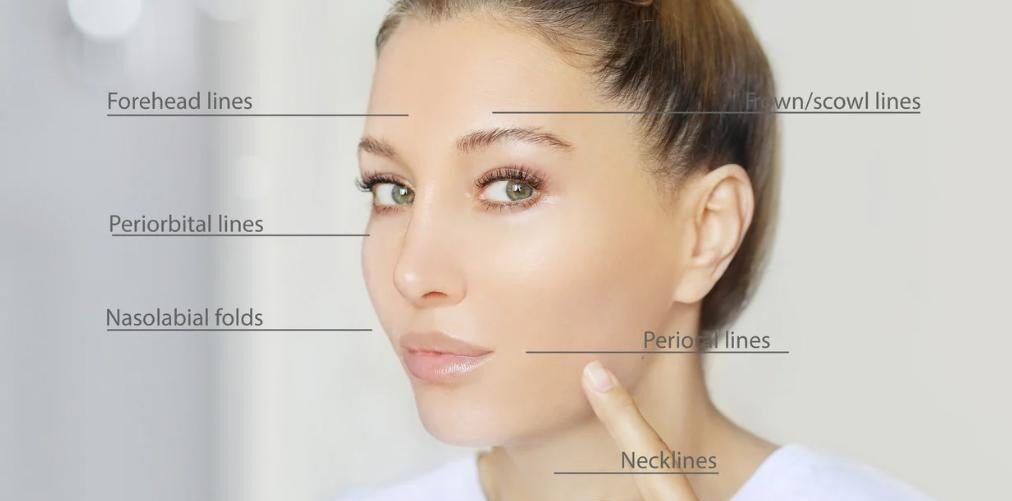
The widespread adoption of dermal fillers in minimally invasive aesthetic procedures has led to a corresponding rise in the incidence and complexity of treatment-related side effects. While early complications were often linked to unregulated practices—resulting in infections, foreign body reactions, and granuloma formation—the growing use of injectable fillers has also brought increased awareness of rare but severe outcomes, such as vascular occlusion, skin necrosis, and blindness.
DERMAL FILLERS – SIDE EFFECTS & ADVERSE EFFECTS
Acute (Immediate or Short-Term) Side Effects: These usually occur within hours to a few days post-injection:
- Swelling
- Redness (Erythema)
- Bruising (Ecchymosis)
- Pain or tenderness at the injection site
- Itching
- Lumps or bumps (palpable or visible)
- Mild bleeding at injection site
- Local hypersensitivity reactions
- Vascular Complications
Vascular complications arising from dermal filler treatments pose significant risks, including ischemia, tissue necrosis, and severe outcomes like blindness and pulmonary embolism. There are two common forms of Vascular complications: extravascular compression and intravascular emboli. Extravascular compression occurs when injected fillers compress adjacent blood vessels, leading to ischemia and potential necrosis, while intravascular emboli result from fillers entering blood vessels, causing blockages.
Note:
- Vascular complications (e.g., vascular occlusion, skin necrosis, or vision loss) are rare but severe and may occur acutely. Immediate recognition and treatment are critical.
Most acute side effects are self-limiting and resolve within a few days.
Chronic (Persistent or Long-Term) Side Effects: These develop or persist weeks to months after treatment:
- Prolonged edema
- Chronic inflammation
- Granuloma formation (foreign body reaction)
- Persistent nodules or lumps
- Tissue fibrosis
- Pigmentation changes (especially in darker skin types)
- Asymmetry or overcorrection
- Migration of filler material
These may require medical intervention such as corticosteroids, hyaluronidase, or surgical excision.
Delayed-Onset Side Effects: These occur weeks to years post-treatment, and are often immune-mediated:
- Delayed inflammatory nodules (may appear months after injection)
- Biofilm-related infections (low-grade infections due to bacterial contamination)
- Late-onset granulomatous reactions
- Filler migration
- Reactivation of herpes simplex virus (if injected near the lips)
May be triggered by systemic infections, vaccinations, or trauma. Treatment involves antibiotics, steroids, or hyaluronidase (for HA fillers).
MANAGEMENT & TREATMENT OF DERMAL FILLER SIDE EFFECTS
Acute Side Effects (Immediate – Hours to Days):
Common acute side effects following dermal filler injections include swelling, redness, bruising, pain, tenderness, itching, mild allergic reactions, bleeding at the injection site, and lumps or bumps. Swelling and redness can be managed effectively with cold compresses, elevation of the treated area, and oral antihistamines if necessary; patients should avoid heat exposure and strenuous exercise during recovery. Bruising may be minimized using topical agents such as Arnica Montana, bromelain, vitamin K cream, cold compresses, and by avoiding NSAIDs before and after treatment. Pain and tenderness can be alleviated with analgesics, preferably acetaminophen, and gentle massage if there is no suspicion of vascular compromise. Mild itching or allergic reactions respond well to oral antihistamines like cetirizine or loratadine and short-term use of topical corticosteroids. Bleeding at the injection site is managed by applying direct pressure for several minutes, ensuring that patients are not on anticoagulant medications prior to treatment. For lumps or bumps, gentle massage within the first 24 to 48 hours is recommended unless the lesions are nodular or inflamed, in which case close observation is warranted.
Chronic Side Effects (Weeks to Months):
Some side effects may develop over weeks or months, including persistent edema or inflammation, nodules or granulomas, asymmetry or overcorrection, filler migration, and pigmentation changes. Persistent swelling or inflammation can be treated with a short course of oral corticosteroids, and referral for imaging such as ultrasound may be considered to evaluate the underlying cause. Nodules or granulomas often require intralesional corticosteroid injections, such as triamcinolone, oral steroids, or in severe cases, surgical excision. Diagnosis may necessitate biopsy to rule out other causes. Asymmetry or overcorrection, especially with hyaluronic acid (HA) fillers, can be addressed by injecting hyaluronidase to dissolve excess product; however, it is advisable to wait at least two weeks before correction unless urgent intervention is needed. Filler migration can also be treated with hyaluronidase for HA-based fillers, while surgical removal may be necessary for non-HA fillers. Pigmentation changes may be managed with topical depigmenting agents like hydroquinone or azelaic acid, with dermatologist referral if the condition persists.
Delayed-Onset Side Effects (Weeks to Years):
Delayed-onset complications include nodules, biofilm infections, late-onset granulomas, and reactivation of herpes simplex virus. Delayed nodules are typically treated empirically with oral antibiotics such as doxycycline or clarithromycin combined with corticosteroids; hyaluronidase should be avoided initially unless there is an active infection. Biofilm infections require combination therapy involving long-term antibiotics, possible drainage, and sometimes hyaluronidase; treatment is ideally guided by culture results. Late-onset granulomas may be managed with intralesional corticosteroids, oral steroids, surgical excision, or immune-modulating medications. Reactivation of herpes simplex virus is treated with oral antivirals such as acyclovir or valacyclovir, and prophylactic antiviral therapy is recommended for patients with a known history of herpes before receiving lip filler treatments.
Emergency – Vascular Compromise (Acute and Severe):
Vascular compromise is a medical emergency characterized by signs such as blanching, pain, dusky or mottled skin, livedo reticularis, and coolness of the affected area. Immediate treatment is critical to prevent tissue necrosis and other serious complications. The first step is to stop the injection immediately, followed by gentle massage of the area and the application of warm compresses to encourage blood flow. High-dose hyaluronidase injections should be administered promptly and may be repeated every 30 to 60 minutes to dissolve hyaluronic acid filler and restore circulation. Additional supportive measures include applying 2% topical nitroglycerin ointment over the ischemic area to promote vasodilation and enhance tissue perfusion, along with oral aspirin to reduce platelet aggregation. Any signs of visual disturbances warrant urgent referral to an ophthalmologist, as retrograde filler migration into the ophthalmic artery can result in irreversible blindness. While these interventions are vital, prevention remains paramount, requiring a thorough understanding of facial vascular anatomy, the use of slow, low-pressure injection techniques, employing cannulas in high-risk zones, and continuous patient monitoring during treatment. Early recognition and rapid intervention significantly improve outcomes and minimize long-term damage. Follow-up care should include monitoring the skin closely for signs of necrosis and secondary infection.
Key Points for Practitioners:
Always conduct a thorough consultation and obtain informed consent before treatment. Use strict aseptic technique, ensure proper injection depth, and aspirate prior to injecting to reduce the risk of vascular compromise. Keep emergency medications such as hyaluronidase, corticosteroids, and antibiotics readily accessible in the Medical clinic. Recognize the signs that require referral to specialists, including dermatologists, infectious disease experts, or oculoplastic surgeons, to ensure timely and appropriate management.
Conclusion:
At Vancoderm Academy, our mission is to equip medical practitioners with the advanced knowledge and clinical skills necessary to perform #dermal_filler treatments safely and effectively. A thorough understanding of both common and serious side effects—including the recognition and management of vascular compromise—is essential for ensuring patient safety and successful outcomes. By emphasizing proper technique, emergency preparedness, and evidence-based practice, we aim to empower practitioners to deliver the highest level of care. By continuing to educate and support healthcare professionals, #Vancoderm_Academy remains committed to raising the standard of education in #aesthetic_medicine.
Thank you for reading—we hope this guide enhances your clinical confidence and supports your continued growth in aesthetic medicine.